OneZero: Sexual Health Apps Can’t Replace Real Sex Talk
Share
What a new service that purports to confirm users are taking HIV prevention medication gets wrong about relationships
Read article in it’s entirety at OneZero.Medium.com…
By Lux Alptraum | April 9, 2019
In I/O, columnist Lux Alptraum explores how technology intersects with sexuality and relationships. I/O will embrace the uncertainty of our future and help us craft a better tomorrow, together.
Back in 1984, during the early days of the HIV epidemic, Armistead Maupin’s novel Babycakes imagined a service that would help people partner up amid the crisis. “How do you let someone you are interested know that YOU ARE SAFE?” Babycakes’ fictional ad copy reads. “Now you can let others know simply by wearing your ‘I’M SAFE’ ring or pendant.”
Now 35 years later, dating with HIV is wildly different. HIV tests have gotten more accurate, enabling doctors to detect positive status within weeks of infection, rather than months. Major advances in treatment have made it possible for HIV+ people to live full, healthy lives. And medications like Truvada (also known as PrEP) help HIV– people have sex with HIV+ partners without fear of infection.
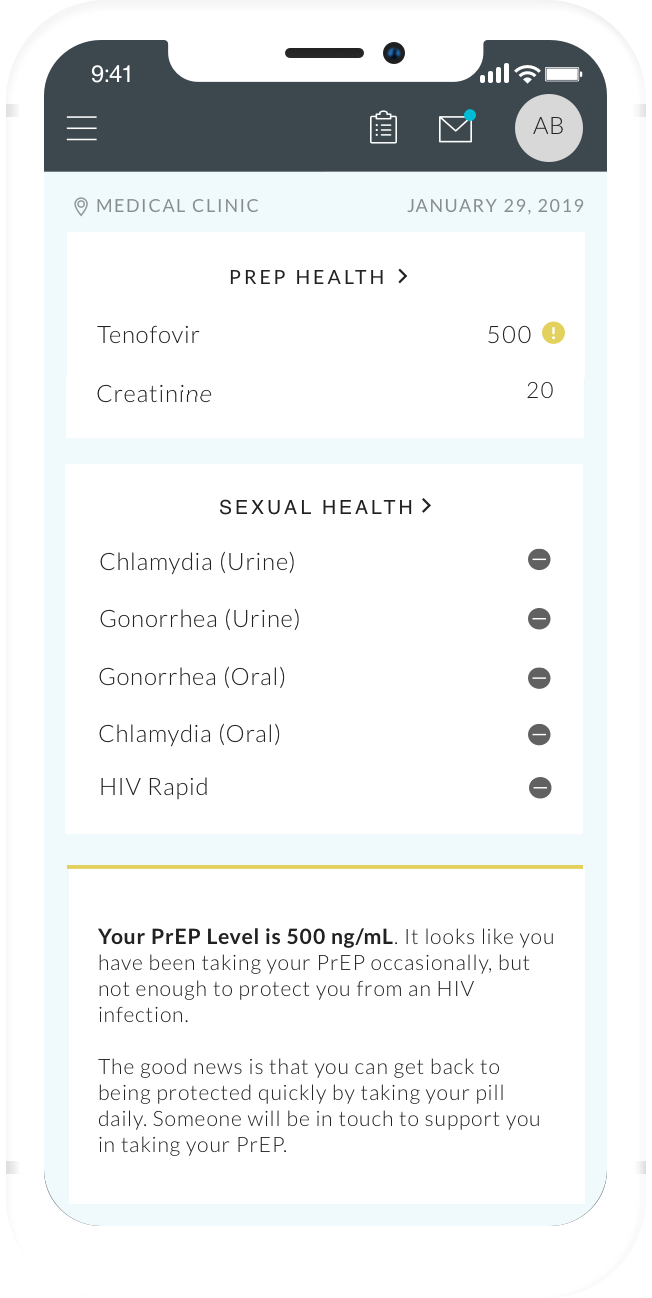
Even with all this progress, however, there’s still a market for products that purport to help people navigate tricky conversations about sexual health—or avoid having them in the first place. UrSure, a urine test that confirms the presence of PrEP in the body, recently partnered with Healthvana, a health app that helps people keep track of their lab results, to offer something of a modern approach to Babycakes’ ring.
“If the purpose [of showing a partner your test results] is that you believe you can further control the situation with another human, you’re doing it wrong.”
“Dating is hard to begin with, and those who have HIV or an STD need to be as careful as those who do not,” the press release declares. “Most sites allow users to self-report they are being treated or are on PrEP for HIV, but how can you prove it to your new date?” The press releases answers its own question in short order, noting that it’s now possible to show potential partners a screenshot from the Healthvana app that “proves” you’re adhering to your medication regimen.
The partnership is hardly surprising in an era where tech has infiltrated every aspect of our daily lives, but the idea is misguided. Granted, there are some significant differences between Babycakes’ring and a time-stamped, physician-certified lab result that confirms PrEP adherence. But both of these sales pitches promise consumers an easy way to outsource a challenging and uncomfortable discussion that everyone needs to have with their potential (or current) sexual partners. Simply put, there is no screenshot-friendly solution to the complicated risks of sex in 2019.
Our susceptibility to these sorts of promises—which have popped up elsewhere, like the “STD-verified” dating app NeatClub—is worth considering more deeply. Decades into the AIDS epidemic, why are people turning to apps to gauge their partners’ trustworthiness? Though our culture feels increasingly open about sex, many of us still have difficulty talking honestly about it, even with someone we’re about to have sex with.
Bryan Stacy, the CEO and co-founder of Biem, an STI testing telemedicine platform, has seen firsthand how quickly users jump on the possibility that technology can help them sidestep challenging conversations. “When we first launched Biem, a lot of people were like, ‘Why don’t you create a dating website with this?’” Stacy tells me over the phone. (He dismisses the notion as “ridiculous.”)
While Stacy does see some value in enabling people to use STI treatment and testing apps to open up conversations with their partners, communication needs to extend beyond the quick flash of a screenshot.
“Anything that’s going to allow that conversation additional validity, additional reason to have the conversation, is good news,” says Stacy. “But—it’s a big but—it is not a proof; it is not a validation of somebody being STI-free. All it is, really, really simply, is proof that somebody is sexually health conscious.
Sexual behavior is far too complicated and unpredictable to be reduced to a single test result.
“If the purpose [of showing a partner your test results] is that you believe you can further control the situation with another human, you’re doing it wrong,” Stacy continues.
As useful as test results can be, they only provide a snapshot of someone’s health rather than an ongoing illustration of their sexual behavior and choices. It may be comforting to think we can ensure our safety just by pulling up a screenshot that confirms that someone has tested negative for an STI or proved compliant with their PrEP regimen, but sexual behavior is far too complicated and unpredictable to be reduced to a single test result.
Yes, knowing that your partner is actually sticking to their daily PrEP routine—and that their urine tests show that the medication is in their system—can be comforting, but that screenshot doesn’t tell you much beyond the fact that they were routinely taking their medication at the time their urine was analyzed. It may not be relevant to the moment you see the screenshot, in other words.
When I chat with Ramin Bastani and Dr. Giffin Daughtridge, respectively the CEOs of Healthvana and UrSure, they’re far more measured about the potential of their products than the press release I received would suggest.
For Daughtridge, the ability to confirm someone’s adherence to PrEP is a powerful tool, enabling people who are on the drug to offer their partners an objective measure of their compliance—something that can feel important when many people who claim to be on PrEP aren’t actually sticking to the regimen. And yet, Daughtridge notes, PrEP requires rigorous adherence to be effective: If you don’t take your pill every day at the same time, you might not be protected. And as a result, last week’s results aren’t any guarantee of continued compliance with one’s medication regimen. At best, UrSure is one part of an ongoing, long-term conversation about sexual health practices—not a permanent guarantee of a partner’s HIV– status.
“It’s better than the status quo,” Bastani says. “A lot of times you have self-reported information,” which can be unreliable, particularly when it comes to something like PrEP adherence. Based on current usage, Bastani is hopeful that the combination of Healthvana and UrSure will enable users to kickstart a conversation about how they’re taking responsibility for their sexual health—rather than shut down the conversation entirely.
Sex and dating will always be fraught with risk and anxiety, and even more so when health concerns are in the mix. But staying safe requires taking responsibility for our own needs, having honest and vulnerable conversations, and allowing ourselves to trust people. There’s no app for that, and it’s unlikely there ever will be.




Follow Us